Cosmetic Surgery Blog
Oral vitamin D rapidly attenuates inflammation from sunburn: an interventional study.

The diverse immunomodulatory effects of vitamin D are increasingly being recognized. However, the ability of oral vitamin D to modulate acute inflammation in vivo has not been established in humans. In a double-blinded, placebo-controlled interventional trial, twenty healthy adults were randomized to receive either placebo or a high dose of vitamin D3 (cholecalciferol) one hour after experimental sunburn induced by an erythemogenic dose of ultraviolet radiation. Compared to placebo, participants receiving vitamin D3 (200,000 IU) demonstrated reduced expression of pro-inflammatory mediators TNF-α (p=0.04) and iNOS (p=0.02) in skin biopsy specimens 48 hours after experimental sunburn. A blinded, unsupervised hierarchical clustering of participants based on global gene expression profiles revealed that participants with significantly higher serum vitamin D3 levels after treatment (p=0.007) demonstrated increased skin expression of the anti-inflammatory mediator arginase-1 (p=0.005), and a sustained reduction in skin redness (p=0.02), correlating with significant expression of genes related to skin barrier repair. In contrast, participants with lower serum vitamin D3 levels had significant expression of pro-inflammatory genes. Together the data may have broad implications for the immunotherapeutic properties of vitamin D in skin homeostasis, and implicate arginase-1 up regulation as a previously unreported mechanism by which vitamin D exerts anti-inflammatory effects in humans.
Click on the link below to find out more:
https://www.ncbi.nlm.nih.gov/pubmed/28576736
Meta-Analysis of the Association Between Phosphodiesterase Inhibitors (PDE5Is) and Risk of Melanoma

Source: https://academic.oup.com/jnci/article-lookup/doi/10.1093/jnci/djx086
The US Food and Drug Administration recently announced the need to evaluate the association between PDE5is and melanoma. We performed a meta-analysis on the association between PDE5i and melanoma using random effects models and examined whether it met Hill’s criteria for causality. A systematic search of Medline, EMBASE, and the Cochrane Library from 1998 to 2016 identified three case-control studies and two cohort studies, including a total of 866 049 men, of whom 41 874 were diagnosed with melanoma. We found a summary estimate indicating an increased risk of melanoma in PDE5i users (relative risk = 1.11, 95% confidence interval = 1.02 to 1.22). However, the association was only statistically significant among men with low PDE5i exposure (not high exposure) and with low-stage melanoma (not high stage), indicating a lack of dose response and biological gradient. PDE5i use was also associated with basal cell cancer, suggesting a lack of specificity and likely confounding by ultraviolet exposure. Thus, although this meta-analysis found a statistically significant association between PDE5i and melanoma, it did not satisfy Hill’s criteria for causality.
Phosphodiesterase inhibitors (PDE5i) are firstline drugs for erectile dysfunction, which is estimated to affect 20% of men age 60 years and older and 30% of men age 70 years and older (1). Phosphodiesterase type 5 is downregulated in BRAF mutations commonly seen in melanoma (2), raising the question of whether pharmacologic inhibition could increase melanoma risk.
In 2014, Li et al. found an association between sildenafil use and melanoma risk (3). Since then, additional studies have been published using large US and European databases (4–6). In 2016, the US Food and Drug Administration placed PDE5i on the watch list of drugs with possible safety issues (7). Our objective was to perform a meta-analysis of published data on the association between PDE5i and melanoma risk. In particular, we sought to determine whether there is an association that meets Hill’s causal criteria including strength, consistency, specificity, temporality, biological gradient, plausibility, coherence, experiment, and analogy (8).
A systematic search was performed using Medline, EMBASE, and the Cochrane Library for publications from 1998 (when PDEI were introduced) to August 2016. The search string was (PDE5 OR phosphodiesterase type 5 OR sildenafil OR tadalafil OR avanafil) AND melanoma (Supplementary Figure 1, available online). From 62 nonduplicate citations screened, four were included in the quantitative synthesis with a moderate to serious risk of bias (Supplementary Table 1, available online) (9).
Data were extracted using a standardized template, including quantitative estimates of the association between PDE5i and melanoma, also stratified by the extent of exposure and melanoma stage. We also examined the association between PDE5i and basal cell carcinoma.
Random effects models were used to calculate summary statistics given the different designs of the included studies. If multiple risk estimates were reported, the multivariable-adjusted estimate was used. Heterogeneity was estimated by use of the chi-square statistic and quantified by use of the I2 values (http://handbook.cochrane.org). All statistical tests were two-sided, and a P value of less than .05 was considered statistically significant.
Three case-control studies and two independent cohort studies were identified including 866 049 men, of whom 41 874 were diagnosed with melanoma. PDE5i users had an increased risk of melanoma (relative risk [RR] = 1.11, 95% confidence interval [CI] = 1.02 to 1.22) (Figure 1). The heterogeneity between studies did not reach statistical significance (I2 = 55.9%, P = .06).
Figure 1.

Association between any, low, and high use of phosphodiesterase inhibitors (PDE5i) and risk of melanoma. A) Any PDE5i exposure. B) Low PDE5i exposure. C) High PDE5i exposure. Low PDE5i exposure was defined in each study as follows: Loeb et al.: one prescription; Matthews et al.: one prescription; Pottegard Danish Nationwide Health Registries (DNHR): fewer than 20 tablets; and Pottegard Kaiser Permanente Northern California (KPNC): fewer than 20 tablets. High PDE5i exposure was defined in the studies as follows: Loeb et al.: six or more prescriptions, Pottegard DNHR: 100 or more tablets; and Pottegard et al. KPNC: 100 or more tablets. The center of each black square is placed at the point estimate; each horizontal line shows the 95% confidence interval (CI) for the estimate for each study. The diamond represents the summary estimate. Statistical weight estimated as for random effect models, accounting for both within-study variance and between-study variance. Test for heterogeneity: A)P = .06, I2 = 55.9%, T2 = 0.0053. B)P = .25, I2 = 27.0%, T2 = 0.0046. C)P = .30, I2 = 18.7%, T2 = 0.0029. All statistical tests were two-sided. Summary risk estimate after exclusion of each respective study: excluding Li et al.: relative risk (RR) = 1.10, 95% CI = 1.02 to 1.19; excluding Loeb: RR = 1.08, 95% CI = 0.98 to 1.19; excluding Matthews: RR = 1.11, 95% CI = 0.99 to 1.25; excluding Pottegard (DNHR): RR = 1.06, 95% CI = 0.96 to 1.18; excluding Pottegard (KPNC): RR = 1.15, 95% CI = 1.04 to 1.26. CI = confidence interval; DNHR = Danish Nationwide Health Registries; KPNC = Kaiser Permanente Northern California; RR = relative risk.
Only low PDE5i exposure was associated with increased risk (RR = 1.15, 95% CI = 1.01 to 1.31), whereas high exposure was not (RR = 1.09, 95% CI = 0.97 to 1.23) (Figure 1). The increase in risk of basal cell carcinoma (RR = 1.16, 95% CI = 1.13 to 1.20) was similar to the increased risk of melanoma (Supplementary Figure 2, available online). Finally, two publications reported stage-specific estimates in three different populations (Figure 2). High PDE5i exposure was associated with an increased risk of stage 0 melanoma (RR = 1.45, 95% CI = 1.09 to 1.92), but decreased risk of stage II to IV melanoma (RR = 0.67, 95% CI = 0.46 to 0.97). Our meta-analysis of four observational studies on PDE5i and melanoma found a statistically significant association. However, it did not meet five of Hill’s nine causal criteria, suggesting against a causal relationship.
Figure 2.

Association between high use of phosphodiesterase inhibitors (PDE5i) and risk of melanoma according to stage. A) In situ melanoma. B) Localized melanoma. C) High-stage melanoma. High PDE5i exposure was defined in the studies as follows: Loeb et al.: six or more prescriptions; Pottegard et al. Danish Nationwide Health Registries (DNHR): 100 or more tablets and Kaiser Permanente Northern California (KPNC): 100 or more tablets. The center of each black square is placed at the point estimate; each horizontal line shows the 95% confidence interval (CI) for the estimate for each study. The diamond represents the summary estimate. Statistical weight estimated as for random effect models, accounting for both within-study variance and between-study variance. Test for heterogeneity: A)P = .98, I2 = 0.0%, T2 = 0. B)P = .37, I2 = 0.0%, T2 = 0. C)P = .93, I2 = 0.0%, T2 = 0. All statistical tests were two-sided. CI = confidence interval; DNHR = Danish Nationwide Health Registries; KPNC = Kaiser Permanente Northern California; RR = relative risk.
The first study on this topic examined 25 848 US health professionals, of which 6% self-reported ever using sildenafil (3). Sildenafil use was statistically significantly associated with melanoma (adjusted hazard ratio [HR] = 1.84, 95% CI = 1.04 to 3.22) but not with other skin cancers. No stage-specific results were reported, sildenafil use was only assessed once, and there were only 14 cases of melanoma among sildenafil users.
The next study used nationwide Swedish registries in Prostate Cancer data Base Sweden (PCBaSe), comparing 4065 melanoma cases with 20 325 age-matched controls (4,10). Overall, 435 cases and 1713 controls were exposed to PDE5i, based on data from the Prescribed Drug Register documenting all prescriptions since July 2005. Although there was an increased overall risk of melanoma among PDE5i users, there was no dose-response relationship, nor an increased risk of high-stage disease. PDE5i users were also statistically significantly more likely to be diagnosed with basal cell skin cancer, indicating a lack of specificity.
Two subsequent studies both used data from the UK Clinical Practice Datalink. Among men with erectile dysfunction, Lian et al. found no statistically significant relationship between PDE5i use with melanoma (328 events/491 478 person-years among PDE5i users vs 112/207 001 person-years in nonusers, adjusted HR = 1.18, 95% CI = 0.95 to 1.47), nor with other skin cancers (5). However, subset analysis found a statistically significantly increased risk of melanoma in men with seven or more PDE5i prescriptions (or ≥ 25 pills) and a statistically significantly increased risk of basal cell cancer with two to five PDE5i prescriptions. Another study by Matthews et al. used the same registry but selected participants based on PDE5i prescriptions (6). Compared with matched controls, PDE5i users had a statistically significantly greater risk of melanoma, basal cell cancer, and solar keratosis, whereas there was no statistically significant association between PDE5i and colorectal cancer, a malignancy not linked to UV exposure. Men with solar keratosis, a proxy for sun exposure, were more likely to use PDE5i subsequently, providing further evidence of sun exposure as a confounder.
Finally, Pottegard et al. performed separate case-control analyses using large registries from Denmark and California (11). In both, they found no statistically significant association between PDE5i ever use or high use and overall melanoma risk. There was also no statistically significant association between PDE5i use and aggressive melanoma. Notably, both PDE5i use and skin cancer are strongly associated with socioeconomic status, suggesting potential for confounding by lifestyle factors. The increased risk of in situ melanoma among PDE5i users and reduction in advanced disease also raises the possibility of detection bias.
Given that PDE5i were placed on the Food and Drug Administration watch list and the recent publication of several large studies, we performed the first meta-analysis on PDE5i and melanoma. Strengths of our study include the large sample size, incorporating data sources from multiple countries. A limitation is that the meta-analysis is based on few estimates and not all included studies provided data on dose response, stage, or other skin cancers, reducing the number of available participants for subset analyses. There is also potential for bias and misclassification of outcome in the primary studies, given the challenges of accurately diagnosing melanoma (particularly in situ melanoma) (12).
In conclusion, a meta-analysis of published studies showed a weak association between PDE5i and melanoma that did not meet Hill’s causal criteria. The lack of dose response, biological gradient, and specificity suggest against a causal relationship. The observed association may be due to confounding from other factors, in particular, sunlight exposure.
Funding
The Swedish Cancer Society 14 0570, the Louis Feil Charitable Lead Trust to SL, and the Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center to SL (P30CA016087).
Note
The funders had no role in the design of the study; the collection, analysis, or interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication.
References
- Bacon CG, Mittleman MA, Kawachi I, et al. Sexual function in men older than 50 years of age: Results from the health professionals follow-up study. Ann Intern Med. 2003;139(3):161–168.Google Scholar CrossRef PubMed
- Arozarena I, Sanchez-Laorden B, Packer L, et al. Oncogenic BRAF induces melanoma cell invasion by downregulating the cGMP-specific phosphodiesterase PDE5A. Cancer Cell. 2011;19(1):45–57.Google Scholar CrossRef PubMed
- Li WQ, Qureshi AA, Robinson KC, et al. Sildenafil use and increased risk of incident melanoma in US men: A prospective cohort study. JAMA Intern Med. 2014;174(6):964–970.Google Scholar CrossRef PubMed
- Loeb S, Folkvaljon Y, Lambe M, et al. Use of phosphodiesterase type 5 inhibitors for erectile dysfunction and risk of malignant melanoma. JAMA. 2015;313(24):2449–2455.Google Scholar CrossRef PubMed
- Lian Y, Yin H, Pollak MN, et al. Phosphodiesterase type 5 inhibitors and the risk of melanoma skin cancer. Eur Urol. 2016;70(5):808–815.Google Scholar CrossRef PubMed
- Matthews A, Langan SM, Douglas IJ, et al. Phosphodiesterase type 5 inhibitors and risk of malignant melanoma: Matched cohort study using primary care data from the UK Clinical Practice Research Datalink. PLoS Med. 2016;13(6):e1002037.Google Scholar CrossRef PubMed
- US Food and Drug Administration FDA Adverse Events Reporting System (FAERS). January–March 2016. http://www.fda.gov/drugs/guidancecomplianceregulatoryinformation/surveillance/adversedrugeffects/ucm509478.htm. Accessed September 22, 2016.
- Hill AB. The environment and disease: Association or causation? Proc R Soc Med. 1965;58:295–300.Google Scholar PubMed
- Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.Google Scholar CrossRef PubMed
- Van Hemelrijck M, Wigertz A, Sandin F, et al. Cohort profile: The National Prostate Cancer Register of Sweden and Prostate Cancer data Base Sweden 2.0. Int J Epidemiol 2013;42(4):956–967.Google Scholar CrossRef PubMed
- Pottegard A, Schmidt SA, Olesen AB, et al. Use of sildenafil or other phosphodiesterase inhibitors and risk of melanoma. Br J Cancer. 2016;115(7):895–900.Google Scholar CrossRef PubMed
- Shoo BA, Sagebiel RW, Kashani-Sabet M. Discordance in the histopathologic diagnosis of melanoma at a melanoma referral center. J Am Acad Dermatol. 2010;62(5):751–756.Google Scholar CrossRef PubMed
© The Author 2017. Published by Oxford University Press.
This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs licence (http://creativecommons.org/licenses/by-nc-nd/4.0/), which permits non-commercial reproduction and distribution of the work, in any medium, provided the original work is not altered or transformed in any way, and that the work is properly cited. For commercial re-use, please contact journals.permissions@oup.com
Supplementary Data
Supplementary Data
– docx file
Basically there were reasons to worry that erectile dysfunction drugs such as Viagra might increase the risk of melanoma.
A new large study published in the Journal of the National Cancer Institute has failed to show any link between the two. They conclude that any previously identified association may be “lifestyle associated”. I guess they speculate that guys who use Viagra are more likely to be tanning!
Brow Lift Santa Monica

The forehead is often the first place many men and women start to notice those first signs of aging. Lines, wrinkles and creases may appear due to loss of volume, loss of elasticity, and gravity that can cause us to look older and more run down than we are. Some people are born with a naturally heavy and drooping brow that cause them to look more severe and even upset when they are just resting. Through Santa Monica Brow Lift Dr. Massey has helped many people achieve the rejuvenated forehead they desired.
The Brow Lift procedure is performed through an incision in the hairline. In some cases the Brow Lift procedure may be performed in combination with other facial rejuvenation procedure such as Blepharoplasty (eyelid lift), Face Lift, Botox or Dermal Fillers. If you are interested in learning more about Brow Lifts and to find out if it may be right for you, contact our office to schedule your consultation with Dr. Massey.
Yet Another Reason to Watch Your Weight

In this study, Fang et al explored the relationship between melanoma outcomes, obesity, and chronic inflammation. Obesity has been associated with development of cancers including melanoma. Adipose tissue produces signaling molecules, such as leptin, which are thought to play a role in cancer progression. Signaling from fat tissue may result in chronic inflammation, as happens in patients with psoriasis, a disease with a well-described relationship to obesity. The authors of this study use C-reactive protein (CRP) as a marker to measure chronic inflammation in patients with melanoma to test whether higher amounts of inflammation result in worse outcomes.
Obese patients in this study had worse overall and melanoma-specific survival. They also had higher CRP levels, which correlated with worse melanoma-specific survival. When the authors controlled for CRP, obesity was no longer an independent risk factor for survival, implying that the reason obese patients did worse was because their adipose tissue was creating a chronic inflammatory state, not that their obesity was independently affecting their mortality.
One limitation of this study was that, although they included 1804 melanoma patients, they only had CRP levels for 725 of them, less than half. Of note, there is a study by Calle et al that examined obesity and mortality associated with many types of cancers and did not detect an increase in melanoma mortality, although that study did not break down melanomas by stage as the Fang study did.1 The relationship between the immune system and melanoma is complex, and, although this study provides correlative evidence for the link between CRP and melanoma mortality, additional studies are warranted to further explain this relationship to better guide recommendations for patients.
Reference
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweigh, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625-1638. http://www.nejm.org/doi/full/10.1056/NEJMoa021423
Sunbeds












Recent study showing that although sun bed use caused a transient increase in vitamine d levels after continued sun bed use vitamin D levels went back down and there was benefit to overall well being.
Although serum vitamin D levels are transiently increased after sunbed use, longer-term increases in serum vitamin D levels are not observed with regular sunbed exposure. Continued sunbed use does not improve serum vitamin D levels nor promote overall well-being.
Message: we know that sun tanning bed use is associated with increased risk of skin cancer. Now we also know that the theoretical benefit in terms of maintaining higher Vitamin D levels is not true.
So there is good reason to avoid it and no good reason to do it!
Click on the link below to find out more of this study.
Incidence and Trends of Basal Cell Carcinoma and Cutaneous Squamous Cell Carcinoma

Article Outline
Patients and Methods
Study Setting
In 2010, Olmsted County had a population of 144,248.20 Although the average socioeconomic status, proportion of college graduates, and proportion of non-Hispanic whites are higher than national averages, epidemiological studies21 in Olmsted County have historically been consistent with national data.
This study was approved by the Mayo Clinic and Olmsted Medical Center institutional review boards. A retrospective population-based cohort was identified through the Rochester Epidemiology Project,22 a research infrastructure (R01-AG034676) that captures health care information for virtually all residents of Olmsted County from 1966 to the present, with 93% of Olmsted County residents seeing any health care provider within the previous 3 years.
Study Criteria
Using the Rochester Epidemiology Project, all medical records were identified for Olmsted County residents who received an International Classification of Diseases, Ninth Revision code diagnosis of 173.00 to 173.99 from January 2, 2000, through December 31, 2010. An NMSC was considered incident if it was a patient’s first BCC or cSCC and was diagnosed during the study period while the patient resided in Olmsted County. A patient could have an incident BCC or cSCC (or both) during the study period. Exclusion criteria included the following: (1) younger than 18 years; (2) cSCC in situ; (3) no BCC or invasive cSCC; (4) previous diagnosis of BCC or cSCC before January 2, 2000; (5) anogenital location; (6) not an Olmsted County resident at the time of incident tumor diagnosis; (7) genetic disorder predisposing to NMSC; (8) previous radiotherapy to the area of tumor formation; and (9) denial of medical record access for research purposes.
Data Collection
Medical records were reviewed by an abstractor (J.G.M. or A.R.S.). The following data were collected: age at diagnosis, sex, race, and previous diagnosis of melanoma. The number of incident tumors, location, size, and histologic subtype were documented for BCC and cSCC, and acantholysis and perineural invasion were documented for cSCC only. For patients with multiple incident tumors, 1 tumor was randomly selected for data collection with a Web-based randomization program.23 Dates were collected for local recurrence, nodal recurrence, distant metastasis, and most recent relevant clinical follow-up with a dermatologist or primary care provider for skin examination. All data were entered into the Research Electronic Data Capture hosted at Mayo Clinic.
Statistical Analyses
Data for BCC and cSCC were analyzed separately. The age- and sex-specific incidence rates (cases per 100,000 person-years) in Olmsted County were calculated, with the numerator being the number of persons who had an incident BCC or cSCC diagnosis and the denominator being the age- and sex-specific counts of the Olmsted County population (from decennial census data and linear interpolation for intercensal years). The rates were adjusted for age and sex according to 2010 US population data; a Poisson error distribution was assumed for 95% CIs. Generalized linear regression models were used to evaluate incidence rates in relation to sex and age (Poisson error distribution was assumed, with crude incidence counts for sex and age groups, offset by the natural logarithm of the number of people).
To facilitate the comparison of incidence estimates for the 2000 to 2010 period with those from earlier periods, previous incidence rates were recalculated after limiting the cases in the previous periods to patients aged 18 years or older and using the total US population structure in 2010 to obtain age- and sex-adjusted estimates. For BCC, incident cases from Rochester were available for the 1976 to 1984 period.18 For cSCC, incident cases from Rochester were available for the 1976 to 1984 and 1984 to 1992 periods and are reported for the 1976 to 1984 and 1985 to 1992 periods.19 In addition, BCC and cSCC incident cases from patients between the ages of 18 and 39 years were available for the 1976 to 1999 period for all of Olmsted County.24 Denominators for each cohort were obtained from the decennial census for Rochester and Olmsted County, with linear interpolation between census years.
Associations between histologic subtype, tumor site, and sex were evaluated using chi-square tests. For the 2000 to 2010 cohort, the duration of follow-up was calculated from the date of the incident BCC or cSCC diagnosis to the date of recurrence or last relevant clinical follow-up. The cumulative incidence of local recurrence was estimated using the Kaplan-Meier method.
All P values were 2-sided; P values less than .05 were considered statistically significant. Statistical analyses were performed with SAS version 9.3 (SAS Institute Inc).
Results
Basal Cell Carcinoma
From 2000 to 2010, 3621 incident BCCs were diagnosed in 3325 patients (mean age at diagnosis, 63.4 years; 50.2% men) (Table 1). The age- and sex-specific incidence rates are listed in Table 2. Incidence rates increased with age in women and at a higher rate in men (P<.001 for sex by age group interaction), with a peak in patients aged 80 to 89 years (Figure 1). Men had a significantly higher age-adjusted incidence rate (360.0 [95% CI, 342.5-377.4] cases per 100,000 person-years) than did women (292.9 [95% CI, 278.6-307.1] cases per 100,000 person-years) (P<.001). The incidence of BCC in patients younger than 40 years was higher in women than in men (Table 2). A previous diagnosis of malignant melanoma or malignant melanoma in situ was recorded for 79 patients (2.4%). The mean age at melanoma diagnosis was 59.7 years; and at subsequent BCC diagnosis, 65.2 years.
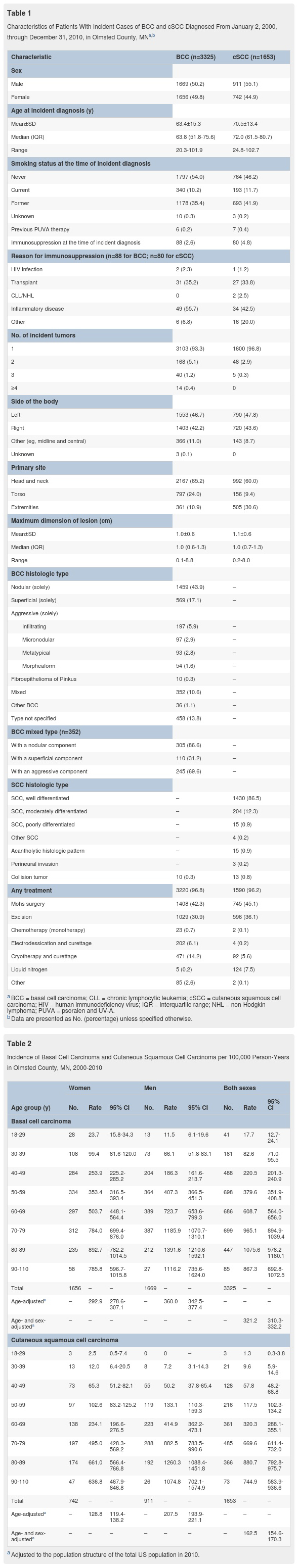
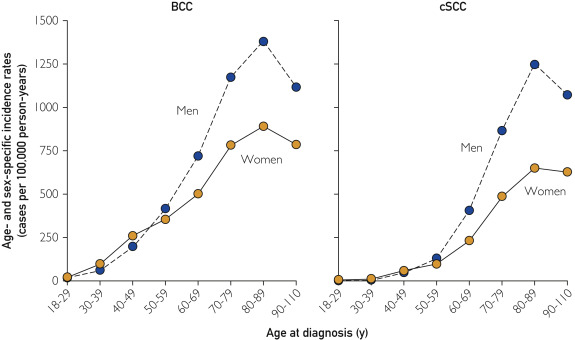
Figure 1
Age- and sex-specific incidence of basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) in Olmsted County, MN, 2000-2010.
The most common locations of BCCs for both sexes were the head and neck followed by the torso (Figure 2). The extremities were the least frequent site, but BCCs occurred in the extremities more commonly in women than in men. The most common histologic subtype was nodular BCC (n=1764 [53.1%]), followed by superficial BCC (n=679 [20.4%]). Men had a statistically higher percentage of the nodular subtype (66.5%) than did women (56.5%) (P<.001). Conversely, women had a statistically higher percentage of the superficial subtype (28.2%) than did men (19.1%) (P<.001). A total of 686 tumors (20.6%) were an aggressive subtype or had an aggressive component (infiltrating, micronodular, metatypical, or morpheaform). Percentages of patients with an aggressive subtype did not differ between women (23.9%) and men (24.0%).
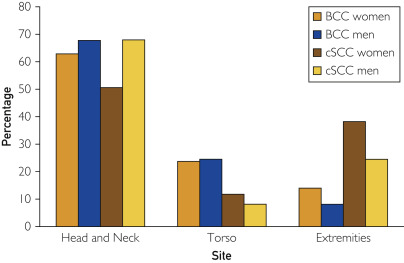
Figure 2
Sites of incident basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) in Olmsted County, MN, 2000-2010. Percentages are based on the number of patients in each subset.
Frequency distributions of BCC subtypes were significantly different depending on tumor location (P<.001). Nodular subtypes were most common on the head and neck (51.3%); superficial subtypes were most common on the extremities (43.2%) and torso (38.8%). Aggressive subtypes accounted for 17.4%, 6.1%, and 5.1% of tumors on the head and neck, extremities, and torso, respectively.
There were 68 recurrences (2.0%), with a median of 3.7 years (interquartile range [IQR], 1.7-5.8 years) between initial BCC diagnosis and recurrence. The median duration of relevant clinical follow-up in patients without a recurrence was 4.9 years (IQR, 1.6-7.9 years). The cumulative incidence of local recurrence of BCC was 0.3%, 1.1%, and 2.2% by 1, 3, and 5 years, respectively, after the incident diagnosis. No distant metastases were recorded.
The incidence of BCC increased in residents older than 18 years between the 1976 to 198418 and 2000 to 2010 periods. The age-adjusted incidence rates increased significantly (P<.001) from 263.2 (95% CI, 232.6-293.8) to 360.0 (95% CI, 342.5-377.4) cases per 100,000 person-years in men and from 189.1 (95% CI, 168.7-209.5) to 292.9 (95% CI, 278.6-307.1) cases per 100,000 person-years in women. The overall age- and sex-adjusted incidence rate increased significantly (P<.001) from 222.0 (95% CI, 204.5-239.5) to 321.2 (95% CI, 310.3-332.2) cases per 100,000 person-years. The increasing incidence of BCC affected both sexes in virtually all age groups
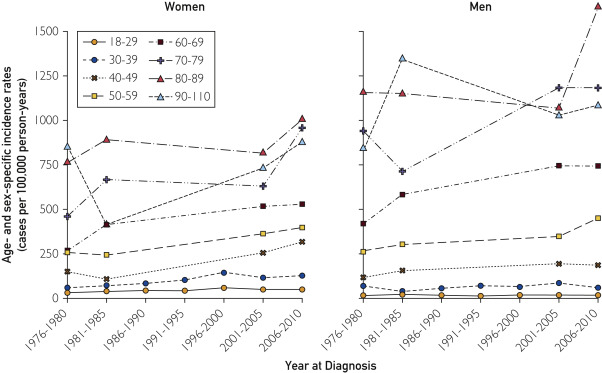
Figure 3
Age- and sex-specific incidence of basal cell carcinoma (BCC) in patients 18 years or older in Olmsted County, MN, 1976-2010. Data were included for all 7 periods for age groups 18-29 and 30-39 years. For all other age groups, data were available for 4 periods: 1976-1980, 1981-1984, 2001-2005, and 2006-2010.
Cutaneous Squamous Cell Carcinoma
From 2000 through 2010, 1711 incident cSCCs were diagnosed in 1653 patients (mean age at diagnosis, 70.5 years; 55.1% men) (Table 1). The age- and sex-specific incidence rates are listed in Table 2. Incidence rates increased with age in women and at a higher rate in men (P<.001 for sex by age group interaction), with a peak in patients aged 80 to 89 years (Figure 1). Men had a significantly higher age-adjusted incidence rate (207.5 [95% CI, 193.9-221.1] cases per 100,000 person-years) than did women (128.8 [95% CI, 119.4-138.2] cases per 100,000 person-years) (P<.001). A previous diagnosis of malignant melanoma or malignant melanoma in situ was recorded for 35 patients (2.1%); most of them were men (n=30; 85.7%). The mean age at melanoma diagnosis was 64.8 years; and at subsequent cSCC diagnosis, 73.1 years.
In men and women, the most common location of cSCC was the head and neck (Figure 2). The second most common location was the extremities, with women (38.1%) having a greater tendency than men (24.4%) to have tumors on the upper and lower extremities (P<.001). The torso was the least likely cSCC location.
There were 31 recurrences (1.9%), with a median of 3.1 years (IQR, 0.7-4.7 years) from cSCC diagnosis to recurrence. The median follow-up in those without a recurrence was 4.4 years (IQR, 1.3-7.5 years). The cumulative incidence of local recurrence after incident cSCC diagnosis was 0.8%, 1.2%, and 2.3% by 1, 3, and 5 years, respectively. Sentinel lymph node biopsy was performed in 2 patients; 1 patient had a positive biopsy result. Four patients had a distant metastasis, and 2 patients had a nodal recurrence; 1 of these patients had both distant metastasis and nodal recurrence.
Since the 1976 to 1984 and 1985 to 1992 periods, the incidence of cSCC has increased in persons older than 18 years.19 In men, the age-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 96.2 (95% CI, 77.1-115.3) in 1976 to 1984, 222.7 (95% CI, 195.2-250.1) in 1985 to 1992, and 207.5 (95% CI, 193.9-221.1) in 2000 to 2010. In women, the age-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 35.3 (95% CI, 26.6-44.0) in 1976 to 1984, 101.9 (95% CI, 87.7-116.0) in 1985 to 1992, and 128.8 (95% CI, 119.4-138.2) in 2000 to 2010. The age- and sex-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 61.8 (95% CI, 52.3-71.4) in 1976 to 1984, 153.7 (95% CI, 139.6-167.7) in 1985 to 1992, and 162.5 (95% CI, 154.6-170.3) in 2000 to 2010. In women, the increase in cSCC incidence over time was statistically significant (P<.001). However, in men, the increase in cSCC incidence was significant between the 1976 to 1984 and 1985 to 1992 periods, with a gradual, nonsignificant decrease by 2000 to 2010.
Discussion
Basal Cell Carcinoma
The overall incidence of BCC increased by 145% between the 1976 to 1984 and 2000 to 2010 periods. However, the increase was not uniform across age groups and sexes. Women in the 40 to 49 age group had the greatest increase in incidence (2.46-fold); women in the 30 to 39 age group had the second greatest increase (1.91-fold). In men, the incidence increased in all age groups except the 18 to 29 group, but the changes were smaller than those in women. A 2013 report25 of BCC incidence in 40- to 50-year-old US health care professionals found that the age-adjusted BCC incidence in women increased from 519 to 1019 cases per 100,000 person-years during the 1986 to 1988 and 2004 to 2006 periods, respectively, and the incidence in men increased from 606 to 1488 cases per 100,000 person-years during the 1988 to 1990 and 2004 to 2006 periods, respectively. Although these incidence rates are markedly higher—and of greater magnitude in men than in women—than the results of the present study when restricted to this age range, they are not derived from a population-based cohort.
In the present study, the anatomical distribution of tumors changed over time. A significantly lower proportion of BCCs were observed on the head and neck during the 2000 to 2010 period (men, 67.6%; women, 62.7%) than during the 1976 to 1984 period (men, 85.9%; women, 83.5%) (P<.001). A significantly higher proportion of BCCs were diagnosed on the torso during the 2000 to 2010 period (men, 24.4%; women, 23.6%) than during the 1976 to 1984 period (men, 10.7%; women, 10.6%) (P<.001). This striking trend is consistent with more recent studies.24, 26, 27, 28, 29, 30, 31 The trends in incidence, anatomical distribution, and tumor subtype may reflect an increase in intermittent recreational UV exposure.31
Cutaneous Squamous Cell Carcinoma
The overall incidence of cSCC increased by 263% between the 1976 to 1984 and 2000 to 2010 periods, which was disproportionately higher than the increase in BCC. In men, the cSCC incidence decreased between the 1985 to 1992 and 2000 to 2010 periods, but in women the incidence increased in many age groups. Women in the 50 to 59 age group had the greatest increase in incidence (1.55-fold); the next greatest increases were in the 70 to 79 (1.52-fold) and 40 to 49 (1.51-fold) age groups. The increasing incidence of BCC at younger ages and of cSCC in older women may reflect tanning habits, which increase the intermittently intense and cumulative UV exposures. A 2012 US study8 estimated the cSCC incidence at 2 different latitudes. The age-adjusted incidence estimates for 2012 in the northern latitude group—most comparable to our cohort—ranged from 46.3 to 134.4 cases per 100,000 person-years in men and from 15.7 to 42.9 cases per 100,000 person-years in women. These estimated incidence rates are significantly lower than the incidence rates in the present study, illustrating the challenge in ascertaining accurate epidemiological data for a relatively common malignancy in the absence of a robust, unified data capture system.
A significant change occurred in the anatomical distribution of cSCC. The proportion of tumors on the extremities increased in men (24.4% in 2000-2010 vs 12.5% in 1976-1984; P=.007) and in women (38.1% in 2000-2010 vs 17.1% in 1976-1984; P<.001). As with BCC, these changes in anatomical distribution were observed in other recent studies10, 11, 32 and may be explained by increased cumulative sun exposure to these anatomical locations.
Younger Populations
For patients younger than 40 years, the increasing incidence of NMSC presents a worrisome trend.24, 33 The incidence rates for both BCC and cSCC were higher in younger women than in younger men in our cohort. These results differ from those of previous studies, in which the incidence rates of cSCC were higher in younger men than in younger women.
Study Limitations
This study has several limitations. First, in this retrospective review, data were derived from documentation of confirmed NMSC, excluding NMSC treated without histologic confirmation. Second, Olmsted County’s location near the 44th parallel and its relatively high proportion of white residents influence the generalizability of the data. Third, the county’s relatively high proportion of college graduates and health care workers may positively influence incidence detection because of increased access to health care.
Conclusion
This study offers robust, comprehensive incidence data on BCC and cSCC from a well-defined population. The incidence of BCC and cSCC in Olmsted County increased between the 2000 and 2010 period as compared with the results of previous population-based studies. The increase in cSCC incidence was disproportionately higher than that in BCC incidence. Women had the greatest increase in incidence rates for both BCC and cSCC, and the anatomical distribution of tumors shifted to the torso for BCC and to the extremities for cSCC. As NMSC incidence rates increase, an emphasis on education, prevention, and surveillance strategies is imperative, and an accurate, accessible national database is needed.
Comparing Melanoma In Situ Treated With Mohs Micrographic Surgery vs. Wide Local Excision

A new article published online in February explores the outcomes of Melanoma In Situ (MIS) when teated with Mohs Micrographic Surgery vs. Wide Local Excision. The take home message from this study is that the Mohs Micrographic Surgery (MMS) is at least as effective as wide local excision (WLE), (with the potential added benefit of possibly sparing more normal tissue that Mohs Micrographic Surgery always offers). The study looked at the results of MMS treated MIS and compared them to the results of WLE treated MIS and found that tumors treated with MMS only recurred at a rate of 5 in 277, versus tumors treated with WLE which reoccurred every 22 in 385. The study was conducted with 662 patients with MIS between 1978 and 2013 with follow up’s performed through 2015. This study is important as MIS is becoming more and more prevalent and WLE is currently the primarily recommended standard of care.
Read more about this study here: https://www.ncbi.nlm.nih.gov/pubmed/28241261
Learn more about Mohs Micrographic Surgery in Santa Monica at Ralph Massey, MD Cosmetic & Skin Cancer Surgery. Contact our office today to schedule your consultation.
Prognostic Role of Histologic Regression in Primary Cutaneous Melanoma

The prognosis for a melanoma is very closely correlated to how deeply it has invaded into the skin (“Breslow Depth”). The for deeper melanomas the risk of spead to lymph nodes is large enough to merit “sentinal node biopsy”. a surgery where radioactive die is injected to tract the first lymphnodes that drain the area of the melanoma, and those nodes are surgically removed to be tested. However some thin melanomas, have signs on pathology indicating they “used to be deeper” but have “regressed” probably becuase the patients immune system has attacked the deper part of the melanoma. No one was sure if the regression was an indication for sentinal node biopsy because we could not be sure how deep the melanoma “used to be”. Or if the regression was a good sign as it indicated an immune respose against the cancer and so sentinal node biopsy was not idicated just because of regression.
This study shows the latter to be the case. So patients with thin melanomas with evidence of “regression” now do not need to worry about “how deep did my melanoma used to be”. They infact have a better prognosis than other patients with thin melanomas becuase thier immune system is putting up a fight!
Click here for the actual article
For years, there has been a running debate regarding the significance of regression. Some articles have reported that regression improved prognosis by reflecting the patient’s enhanced immune response and therefore ability to fight the malignancy. Others implied that prognosis was likely made worse when regression was identified because the actual depth of the melanoma could no longer be accurately measured and was almost certainly deeper.
This collaborative review from Italy culled the literature to attempt to finally establish the prognostic significance of histologic regression in primary melanoma. Using various search engines, they reviewed 1876 articles published from January 1966 through August 2015 that dealt with regression. Due to strict criteria, only 10 studies were eligible to be included in their analysis. These 10 studies included 8557 patients. Their meta-analysis revealed that patients who demonstrated histologic regression in their primary melanoma had a lower likelihood of death, allowing the authors to conclude that histologic regression is a protective feature for survival.
This conclusion is extremely important. It will finally resolve and stop the performance of sentinel lymph node biopsies in those patients with a thin melanoma because of the presence of regression. However, this retrospective study based on observational studies has limitations and potential flaws, including but not limited to, the heterogeneity of the melanoma features (ulceration, thickness) in the studies reviewed, the confounding impact of meta-regression, the different definitions of histologic regression in the various studies, and the lack of information regarding the percentage of the lesion that was regressed.
Melanoma is an immunogenic tumor, and therefore it is not surprising that regression, due to the host response, would be associated with an improved prognosis. Nonetheless, additional studies with an agreed-upon definition of regression are needed to confirm these results.
Written by Jane Grant-Kels MD
Anti-Aging Gene Identified in Melanoma Treatment

At The Wistar Institute in Philadelphia researchers have discovered that an anti-diabetic drug stimulates an anti-aging gene which has the ability to restrain the progress of melanoma in older people. Melanoma is a common form of skin cancer that is seen more frequently in patients who are older. While target therapies being used currently to treat this form of skin cancer have had better survival rates than chemotherapy, they are also limited if the patient develops a resistance to them. In the researchers latest study, they discovered that by treating mice with Klotho promoting drug, the mice’s Wnt5A levels (which promote metastatic progression and resistance to therapy) were lowered and their therapy-resistant melanoma decreased…but this result only occurred in the older mice, not the young mice.
Ashani Weeraatna, Ph.D. stated that the new study indicated a “differential therapeutic approach can be beneficial for older patients in melanoma and suggests that age should be taken into account to design better treatments for certain cohorts of patients.”
“We believe that there is a threshold effect whereby the levels of Klotho, dictated mostly by the age of the patients, are crucial in determining whether they will benefit from this treatment or not,” Reeti Behera, Ph.D., added.
Learn more what Melanoma looks like, what causes it, and how it can be prevented.
The Impact of Mindfulness in Dermatology

“Mindfulness” is defined as “a mental state achieved by focusing one’s awareness on the present moment, while calmly acknowledging and accepting one’s feelings, thoughts, and bodily sensations, used as a therapeutic technique.” Recently, The National Center for Biotechnology Information (NCBI) published a study on “the importance of mindfulness in psychosocial distress and quality of life in dermatology patients.” They found that those with chronic dermatological issues often had higher rates of anxiety and depression than the rest of the populace, as well as a decreased quality of life. Their objective was to determine the connection between psychosocial anxiety and mindfulness in these patients. The study was conducted in the United Kingdom with adults who had clearly visible dermatological issues.
Participants of the study then completed questionnaires which aimed to asses the severity of their disease, their quality of life, depression, anxiety and mindfulness. They found that significant social anxiety was present in 33.4% of the participants and that 26.7% stated their skin condition had a large, direct impact on their quality of life. Perhaps unsurprisingly, participants with more visible and severe skin conditions felt high levels of distress. However, participants who had higher levels of mindfulness (meaning they were more presently aware and practiced nonjudgmental thinking) experienced lower levels of distress, whether they had a more severe skin condition or note.
The reviewers therefore concluded that therapy techniques such as cognitive behavior therapy, habit reversal, and mindfulness can be a beneficial practice for physical and patients in the dermatology field.
