Incidence and Trends of Basal Cell Carcinoma and Cutaneous Squamous Cell Carcinoma

Article Outline
Patients and Methods
Study Setting
In 2010, Olmsted County had a population of 144,248.20 Although the average socioeconomic status, proportion of college graduates, and proportion of non-Hispanic whites are higher than national averages, epidemiological studies21 in Olmsted County have historically been consistent with national data.
This study was approved by the Mayo Clinic and Olmsted Medical Center institutional review boards. A retrospective population-based cohort was identified through the Rochester Epidemiology Project,22 a research infrastructure (R01-AG034676) that captures health care information for virtually all residents of Olmsted County from 1966 to the present, with 93% of Olmsted County residents seeing any health care provider within the previous 3 years.
Study Criteria
Using the Rochester Epidemiology Project, all medical records were identified for Olmsted County residents who received an International Classification of Diseases, Ninth Revision code diagnosis of 173.00 to 173.99 from January 2, 2000, through December 31, 2010. An NMSC was considered incident if it was a patient’s first BCC or cSCC and was diagnosed during the study period while the patient resided in Olmsted County. A patient could have an incident BCC or cSCC (or both) during the study period. Exclusion criteria included the following: (1) younger than 18 years; (2) cSCC in situ; (3) no BCC or invasive cSCC; (4) previous diagnosis of BCC or cSCC before January 2, 2000; (5) anogenital location; (6) not an Olmsted County resident at the time of incident tumor diagnosis; (7) genetic disorder predisposing to NMSC; (8) previous radiotherapy to the area of tumor formation; and (9) denial of medical record access for research purposes.
Data Collection
Medical records were reviewed by an abstractor (J.G.M. or A.R.S.). The following data were collected: age at diagnosis, sex, race, and previous diagnosis of melanoma. The number of incident tumors, location, size, and histologic subtype were documented for BCC and cSCC, and acantholysis and perineural invasion were documented for cSCC only. For patients with multiple incident tumors, 1 tumor was randomly selected for data collection with a Web-based randomization program.23 Dates were collected for local recurrence, nodal recurrence, distant metastasis, and most recent relevant clinical follow-up with a dermatologist or primary care provider for skin examination. All data were entered into the Research Electronic Data Capture hosted at Mayo Clinic.
Statistical Analyses
Data for BCC and cSCC were analyzed separately. The age- and sex-specific incidence rates (cases per 100,000 person-years) in Olmsted County were calculated, with the numerator being the number of persons who had an incident BCC or cSCC diagnosis and the denominator being the age- and sex-specific counts of the Olmsted County population (from decennial census data and linear interpolation for intercensal years). The rates were adjusted for age and sex according to 2010 US population data; a Poisson error distribution was assumed for 95% CIs. Generalized linear regression models were used to evaluate incidence rates in relation to sex and age (Poisson error distribution was assumed, with crude incidence counts for sex and age groups, offset by the natural logarithm of the number of people).
To facilitate the comparison of incidence estimates for the 2000 to 2010 period with those from earlier periods, previous incidence rates were recalculated after limiting the cases in the previous periods to patients aged 18 years or older and using the total US population structure in 2010 to obtain age- and sex-adjusted estimates. For BCC, incident cases from Rochester were available for the 1976 to 1984 period.18 For cSCC, incident cases from Rochester were available for the 1976 to 1984 and 1984 to 1992 periods and are reported for the 1976 to 1984 and 1985 to 1992 periods.19 In addition, BCC and cSCC incident cases from patients between the ages of 18 and 39 years were available for the 1976 to 1999 period for all of Olmsted County.24 Denominators for each cohort were obtained from the decennial census for Rochester and Olmsted County, with linear interpolation between census years.
Associations between histologic subtype, tumor site, and sex were evaluated using chi-square tests. For the 2000 to 2010 cohort, the duration of follow-up was calculated from the date of the incident BCC or cSCC diagnosis to the date of recurrence or last relevant clinical follow-up. The cumulative incidence of local recurrence was estimated using the Kaplan-Meier method.
All P values were 2-sided; P values less than .05 were considered statistically significant. Statistical analyses were performed with SAS version 9.3 (SAS Institute Inc).
Results
Basal Cell Carcinoma
From 2000 to 2010, 3621 incident BCCs were diagnosed in 3325 patients (mean age at diagnosis, 63.4 years; 50.2% men) (Table 1). The age- and sex-specific incidence rates are listed in Table 2. Incidence rates increased with age in women and at a higher rate in men (P<.001 for sex by age group interaction), with a peak in patients aged 80 to 89 years (Figure 1). Men had a significantly higher age-adjusted incidence rate (360.0 [95% CI, 342.5-377.4] cases per 100,000 person-years) than did women (292.9 [95% CI, 278.6-307.1] cases per 100,000 person-years) (P<.001). The incidence of BCC in patients younger than 40 years was higher in women than in men (Table 2). A previous diagnosis of malignant melanoma or malignant melanoma in situ was recorded for 79 patients (2.4%). The mean age at melanoma diagnosis was 59.7 years; and at subsequent BCC diagnosis, 65.2 years.
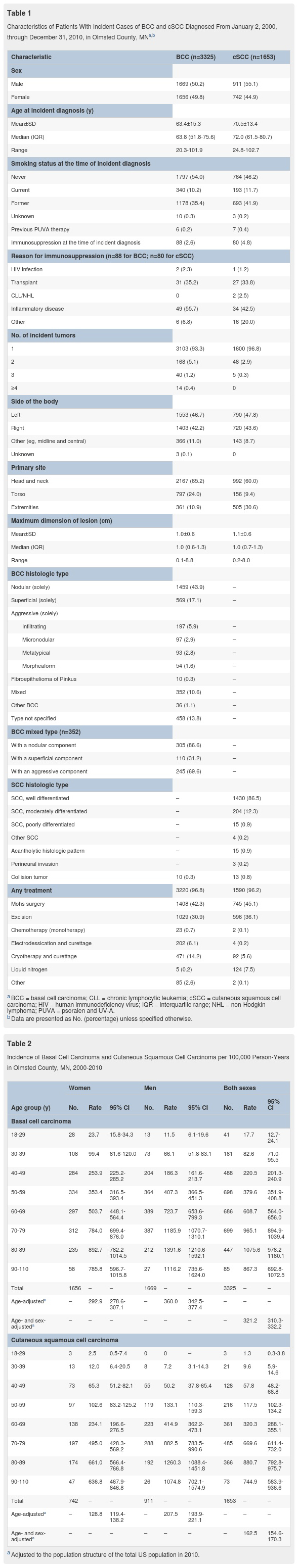
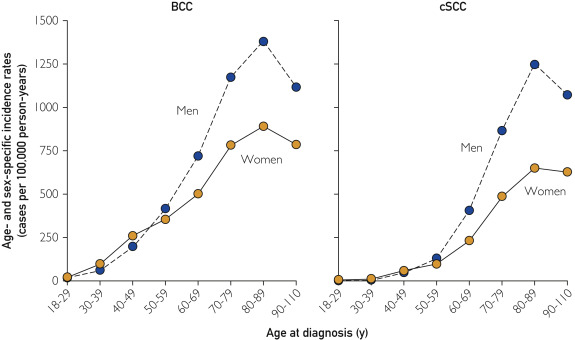
Figure 1
Age- and sex-specific incidence of basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) in Olmsted County, MN, 2000-2010.
The most common locations of BCCs for both sexes were the head and neck followed by the torso (Figure 2). The extremities were the least frequent site, but BCCs occurred in the extremities more commonly in women than in men. The most common histologic subtype was nodular BCC (n=1764 [53.1%]), followed by superficial BCC (n=679 [20.4%]). Men had a statistically higher percentage of the nodular subtype (66.5%) than did women (56.5%) (P<.001). Conversely, women had a statistically higher percentage of the superficial subtype (28.2%) than did men (19.1%) (P<.001). A total of 686 tumors (20.6%) were an aggressive subtype or had an aggressive component (infiltrating, micronodular, metatypical, or morpheaform). Percentages of patients with an aggressive subtype did not differ between women (23.9%) and men (24.0%).
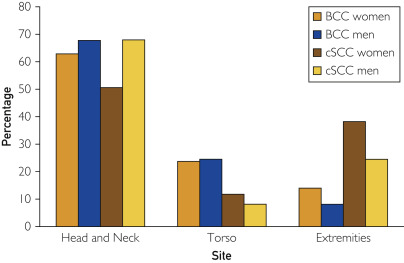
Figure 2
Sites of incident basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC) in Olmsted County, MN, 2000-2010. Percentages are based on the number of patients in each subset.
Frequency distributions of BCC subtypes were significantly different depending on tumor location (P<.001). Nodular subtypes were most common on the head and neck (51.3%); superficial subtypes were most common on the extremities (43.2%) and torso (38.8%). Aggressive subtypes accounted for 17.4%, 6.1%, and 5.1% of tumors on the head and neck, extremities, and torso, respectively.
There were 68 recurrences (2.0%), with a median of 3.7 years (interquartile range [IQR], 1.7-5.8 years) between initial BCC diagnosis and recurrence. The median duration of relevant clinical follow-up in patients without a recurrence was 4.9 years (IQR, 1.6-7.9 years). The cumulative incidence of local recurrence of BCC was 0.3%, 1.1%, and 2.2% by 1, 3, and 5 years, respectively, after the incident diagnosis. No distant metastases were recorded.
The incidence of BCC increased in residents older than 18 years between the 1976 to 198418 and 2000 to 2010 periods. The age-adjusted incidence rates increased significantly (P<.001) from 263.2 (95% CI, 232.6-293.8) to 360.0 (95% CI, 342.5-377.4) cases per 100,000 person-years in men and from 189.1 (95% CI, 168.7-209.5) to 292.9 (95% CI, 278.6-307.1) cases per 100,000 person-years in women. The overall age- and sex-adjusted incidence rate increased significantly (P<.001) from 222.0 (95% CI, 204.5-239.5) to 321.2 (95% CI, 310.3-332.2) cases per 100,000 person-years. The increasing incidence of BCC affected both sexes in virtually all age groups
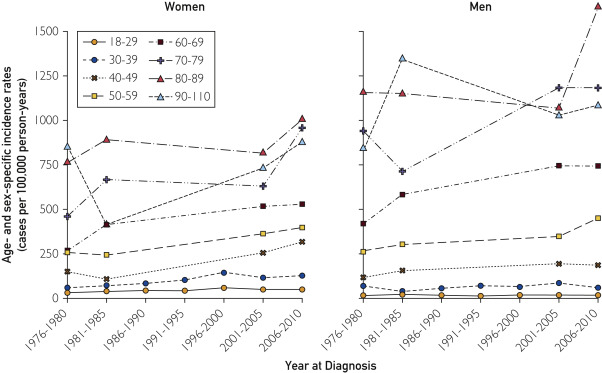
Figure 3
Age- and sex-specific incidence of basal cell carcinoma (BCC) in patients 18 years or older in Olmsted County, MN, 1976-2010. Data were included for all 7 periods for age groups 18-29 and 30-39 years. For all other age groups, data were available for 4 periods: 1976-1980, 1981-1984, 2001-2005, and 2006-2010.
Cutaneous Squamous Cell Carcinoma
From 2000 through 2010, 1711 incident cSCCs were diagnosed in 1653 patients (mean age at diagnosis, 70.5 years; 55.1% men) (Table 1). The age- and sex-specific incidence rates are listed in Table 2. Incidence rates increased with age in women and at a higher rate in men (P<.001 for sex by age group interaction), with a peak in patients aged 80 to 89 years (Figure 1). Men had a significantly higher age-adjusted incidence rate (207.5 [95% CI, 193.9-221.1] cases per 100,000 person-years) than did women (128.8 [95% CI, 119.4-138.2] cases per 100,000 person-years) (P<.001). A previous diagnosis of malignant melanoma or malignant melanoma in situ was recorded for 35 patients (2.1%); most of them were men (n=30; 85.7%). The mean age at melanoma diagnosis was 64.8 years; and at subsequent cSCC diagnosis, 73.1 years.
In men and women, the most common location of cSCC was the head and neck (Figure 2). The second most common location was the extremities, with women (38.1%) having a greater tendency than men (24.4%) to have tumors on the upper and lower extremities (P<.001). The torso was the least likely cSCC location.
There were 31 recurrences (1.9%), with a median of 3.1 years (IQR, 0.7-4.7 years) from cSCC diagnosis to recurrence. The median follow-up in those without a recurrence was 4.4 years (IQR, 1.3-7.5 years). The cumulative incidence of local recurrence after incident cSCC diagnosis was 0.8%, 1.2%, and 2.3% by 1, 3, and 5 years, respectively. Sentinel lymph node biopsy was performed in 2 patients; 1 patient had a positive biopsy result. Four patients had a distant metastasis, and 2 patients had a nodal recurrence; 1 of these patients had both distant metastasis and nodal recurrence.
Since the 1976 to 1984 and 1985 to 1992 periods, the incidence of cSCC has increased in persons older than 18 years.19 In men, the age-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 96.2 (95% CI, 77.1-115.3) in 1976 to 1984, 222.7 (95% CI, 195.2-250.1) in 1985 to 1992, and 207.5 (95% CI, 193.9-221.1) in 2000 to 2010. In women, the age-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 35.3 (95% CI, 26.6-44.0) in 1976 to 1984, 101.9 (95% CI, 87.7-116.0) in 1985 to 1992, and 128.8 (95% CI, 119.4-138.2) in 2000 to 2010. The age- and sex-adjusted incidence rates (cases per 100,000 person-years) increased as follows: 61.8 (95% CI, 52.3-71.4) in 1976 to 1984, 153.7 (95% CI, 139.6-167.7) in 1985 to 1992, and 162.5 (95% CI, 154.6-170.3) in 2000 to 2010. In women, the increase in cSCC incidence over time was statistically significant (P<.001). However, in men, the increase in cSCC incidence was significant between the 1976 to 1984 and 1985 to 1992 periods, with a gradual, nonsignificant decrease by 2000 to 2010.
Discussion
Basal Cell Carcinoma
The overall incidence of BCC increased by 145% between the 1976 to 1984 and 2000 to 2010 periods. However, the increase was not uniform across age groups and sexes. Women in the 40 to 49 age group had the greatest increase in incidence (2.46-fold); women in the 30 to 39 age group had the second greatest increase (1.91-fold). In men, the incidence increased in all age groups except the 18 to 29 group, but the changes were smaller than those in women. A 2013 report25 of BCC incidence in 40- to 50-year-old US health care professionals found that the age-adjusted BCC incidence in women increased from 519 to 1019 cases per 100,000 person-years during the 1986 to 1988 and 2004 to 2006 periods, respectively, and the incidence in men increased from 606 to 1488 cases per 100,000 person-years during the 1988 to 1990 and 2004 to 2006 periods, respectively. Although these incidence rates are markedly higher—and of greater magnitude in men than in women—than the results of the present study when restricted to this age range, they are not derived from a population-based cohort.
In the present study, the anatomical distribution of tumors changed over time. A significantly lower proportion of BCCs were observed on the head and neck during the 2000 to 2010 period (men, 67.6%; women, 62.7%) than during the 1976 to 1984 period (men, 85.9%; women, 83.5%) (P<.001). A significantly higher proportion of BCCs were diagnosed on the torso during the 2000 to 2010 period (men, 24.4%; women, 23.6%) than during the 1976 to 1984 period (men, 10.7%; women, 10.6%) (P<.001). This striking trend is consistent with more recent studies.24, 26, 27, 28, 29, 30, 31 The trends in incidence, anatomical distribution, and tumor subtype may reflect an increase in intermittent recreational UV exposure.31
Cutaneous Squamous Cell Carcinoma
The overall incidence of cSCC increased by 263% between the 1976 to 1984 and 2000 to 2010 periods, which was disproportionately higher than the increase in BCC. In men, the cSCC incidence decreased between the 1985 to 1992 and 2000 to 2010 periods, but in women the incidence increased in many age groups. Women in the 50 to 59 age group had the greatest increase in incidence (1.55-fold); the next greatest increases were in the 70 to 79 (1.52-fold) and 40 to 49 (1.51-fold) age groups. The increasing incidence of BCC at younger ages and of cSCC in older women may reflect tanning habits, which increase the intermittently intense and cumulative UV exposures. A 2012 US study8 estimated the cSCC incidence at 2 different latitudes. The age-adjusted incidence estimates for 2012 in the northern latitude group—most comparable to our cohort—ranged from 46.3 to 134.4 cases per 100,000 person-years in men and from 15.7 to 42.9 cases per 100,000 person-years in women. These estimated incidence rates are significantly lower than the incidence rates in the present study, illustrating the challenge in ascertaining accurate epidemiological data for a relatively common malignancy in the absence of a robust, unified data capture system.
A significant change occurred in the anatomical distribution of cSCC. The proportion of tumors on the extremities increased in men (24.4% in 2000-2010 vs 12.5% in 1976-1984; P=.007) and in women (38.1% in 2000-2010 vs 17.1% in 1976-1984; P<.001). As with BCC, these changes in anatomical distribution were observed in other recent studies10, 11, 32 and may be explained by increased cumulative sun exposure to these anatomical locations.
Younger Populations
For patients younger than 40 years, the increasing incidence of NMSC presents a worrisome trend.24, 33 The incidence rates for both BCC and cSCC were higher in younger women than in younger men in our cohort. These results differ from those of previous studies, in which the incidence rates of cSCC were higher in younger men than in younger women.
Study Limitations
This study has several limitations. First, in this retrospective review, data were derived from documentation of confirmed NMSC, excluding NMSC treated without histologic confirmation. Second, Olmsted County’s location near the 44th parallel and its relatively high proportion of white residents influence the generalizability of the data. Third, the county’s relatively high proportion of college graduates and health care workers may positively influence incidence detection because of increased access to health care.
Conclusion
This study offers robust, comprehensive incidence data on BCC and cSCC from a well-defined population. The incidence of BCC and cSCC in Olmsted County increased between the 2000 and 2010 period as compared with the results of previous population-based studies. The increase in cSCC incidence was disproportionately higher than that in BCC incidence. Women had the greatest increase in incidence rates for both BCC and cSCC, and the anatomical distribution of tumors shifted to the torso for BCC and to the extremities for cSCC. As NMSC incidence rates increase, an emphasis on education, prevention, and surveillance strategies is imperative, and an accurate, accessible national database is needed.
